I am an assistant professor in the Department of Anesthesiology at the Duke University School of Medicine. My background is in human factors engineering, and I conduct research aimed at improving patient safety. The goal of one of my studies is to reduce the time it takes to respond to cardiac arrest in the hospital. My colleague Dr. Melanie Wright, from Trinity Health, and I use iCoda to collect data for this study.
If you don't have a Vosaic account for recording simulations and conducting video-based debriefs (iCoda's replacement), you can start with a free trial today.
Hospitalized patients who are at risk for cardiac arrest and other arrhythmias are put on telemetry to continuously monitor their heart rhythm. A telemetry monitor is a portable box that is attached to the patient’s ECG leads and displays his or her heart rate and rhythm at a central station. The monitor sends an alarm when it detects an abnormal rhythm, notifying the person monitoring the patient to check on the patient (Figure 1). A quick and efficient response to cardiac arrest is critical in order to increase the patient’s chance of survival. Continuous ECG telemetry can be implemented with local (on the care unit) or remote monitoring stations. In many hospitals, watchers are dedicated nurses or technicians who monitor a bank of displays


There are several factors thought to affect response times to a patient undergoing cardiac arrest, including the number of patients watchers are assigned to monitor and the method they use to notify the patient’s nurse.
We set out to compare 6 telemetry monitoring methods that implement these and other factors in different ways, to determine the method that will lead to the quickest response to critical heart rhythms. To compare the methods, we are building computer models that simulate monitor watchers’ and unit nurses’ work, including such factors as watchers’ response rates to false alarms and nurses’ time to reach patients.
To collect the data that will ‘feed’ into the computer models, we are conducting observations, interviews, and cardiac arrhythmia simulations in central monitoring stations and nursing units.
Monitor Watcher Observations
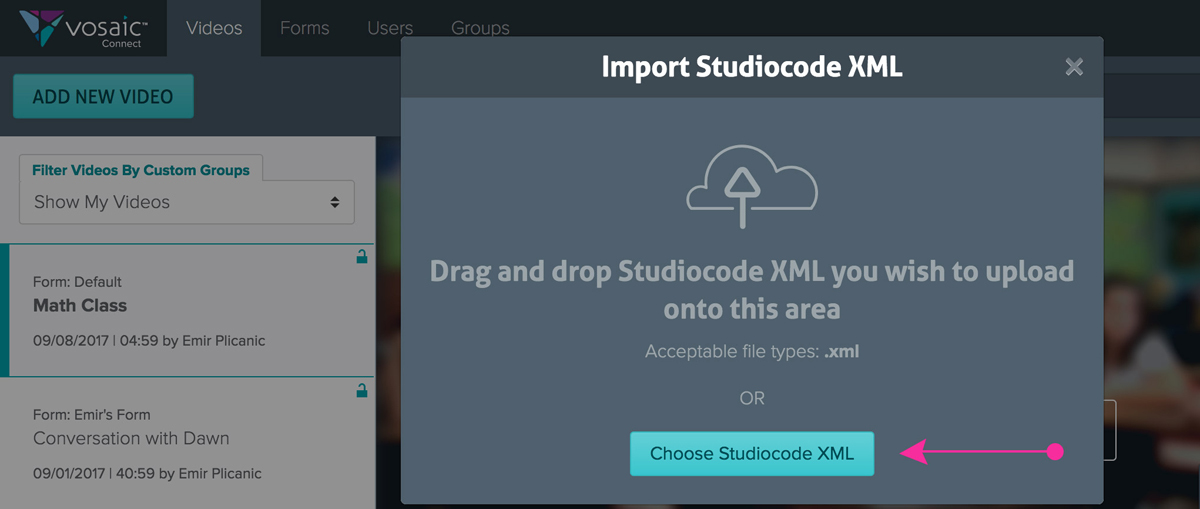
We first tried to observe monitor watchers using paper-based data collection sheets, but we quickly realized that writing down the times different patients’ alarms went off, the types of alarms, and how watchers responded to them was an overwhelming task, particularly when watchers monitored a large volume of patients. We then looked into software development of a mobile app that would allow us to automate data collection, but this solution was cost-prohibitive and would limit our ability to make changes to the app as our needs evolved. We had previously used Studiocode in other research projects, and that’s how we found out about another Vosaic product, iCoda, which would allow us to develop and modify data collection forms in-house at much lower cost.
Using iCoda, we designed a form that an observer can use to collect data about a watcher monitoring up to 32 patients at a time (Figure 3). When a patient’s alarm goes off, the observer indicates the alarm type – crisis, warning, or advisory. For crisis and warning alarms, the observer selects the reason for the alarm, e.g., turning the ECG monitor off (‘Standby’). The observer also selects what the watcher did in response to the alarm, e.g., call the patient’s unit (Figure 4).


Nurse Observations
We also automated the process for collecting data about nurses’ task distribution and travel time between tasks.


Summary
iCoda has been a very useful tool in our research project. The data we are collecting is being used to develop computer simulation models of different monitoring methods. The models will allow us to compare the methods and to determine which is the most effective in reducing response times to cardiac arrest. They will also allow us to determine optimal values for parameters that affect these response times.
Important Update: 01/2019
Since this article was published, both iCoda and Studiocode have been sunset, and replaced with our cloud-based product.